Fungal infections can be very harmful. And one of them in particular – mucormycosis has increased the severity of suffering in a country already affected by Covid-19. According to some reports from India, some patients with Covid or those who are recovering have found signs of an infection called “black fungus”.
As of March this year, 41 cases of Covid-19-associated mucormycosis have been confirmed worldwide, 70% of which have been reported in India. Also the number of cases is much higher, which is not surprising given the current wave of Covid-19 infections in India.
But what is mucormycosis, and what is its Covid-19 binding?
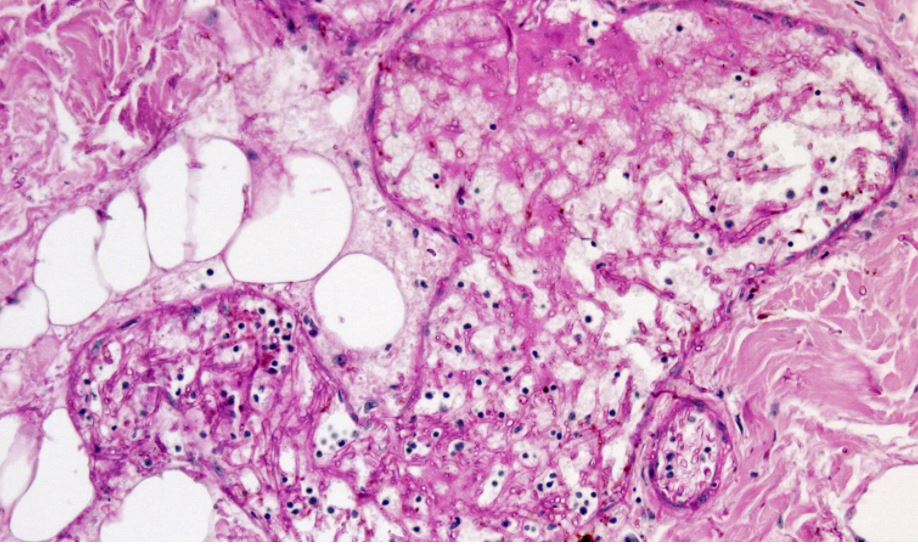
Mucormycosis, formerly known as zygomycosis, is a disease caused by fungi belonging to the “Mucorales” fungus family. Mushrooms in this family are usually found in the soil. They are responsible for infections in humans called Rhizopus oryzae. In India however, Apophysomyces, found in tropical and subtropical climates, is also very common, reports abcnews.al
In the laboratory, these mushrooms develop rapidly and have a blackish brown color. Those that cause disease in humans develop at body temperature and in acidic environments.
How can we become infected with mucormycosis?
The fungus in the Mucorales family is considered opportunistic, meaning that it usually infects people who have a weak immune system. The use of medications such as corticosteroids can damage the immune system as well as a number of other conditions like cancer or transplanted.
There are three ways people can become infected with mucormycosis – by taking spores from food or medicine, or when the spores contaminate wounds. We actually get spores of a lot of fungi every day. But our immune system and lungs, if healthy prevent them from causing an infection.
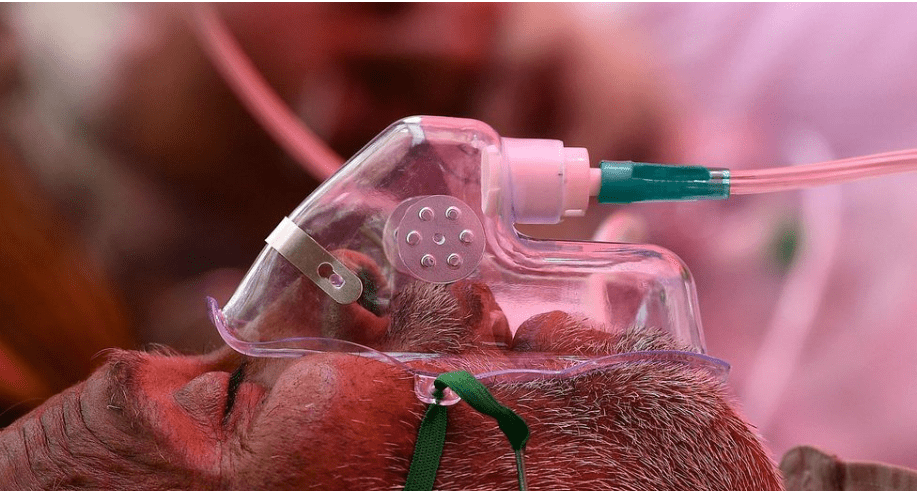
When our lungs are damaged and our immune system is weak, as is the case in critically ill patients with Covid, these spores can attach to the airways and invade our body tissues.
Mucormycosis can occur in the lungs, but the nose and sinuses are the most common site of mucormycosis infection. From there it can spread to the eyes, causing blindness, or to the brain, causing headaches.
It can also spread to the skin. Life-threatening wound infections have been observed after injuries during natural disasters or on battlefields where wounds have been contaminated by soil and water.
In the environment
There have been very few mucormycosis infections in countries other than India. So why are these infections spreading in India?
Prior to the pandemic, mucormycosis was a very common infection in India compared to any other country. The infection affects 14 per 100,000 people in India compared to 0.06 per 100,000 in Australia.
Globally, mucormycosis outbreaks have occurred due to contaminated products such as hospital lines, medicines, and packaged foods. But the spread of mucormycosis in India shows that the spread of infection does not come from a single contaminated source.
According to the data 94% of patients who were infected with mucormycosis had diabetes. Mucorales can be found in soil, rotten food, bird and animal feces, water and air around construction sites, and humid environments. When diabetes is not well controlled blood sugar is high and tissues become acidic – a good environment for the growth of Mucorales fungi.
Of all the cases of mucormycosis published in scientific journals globally between 2000-2017, diabetes accounted for 40% of cases.
People with diabetes and overweight tend to develop more severe symptoms of Covid-19. This means that they are more likely to take corticosteroids, which are often used to treat Covid-19. But corticosteroids – along with diabetes increase the risk of mucormycosis, reports abcnews.al
Meanwhile, the virus that causes Covid-19 can damage the tissues of the airways and blood vessels, which can also increase the susceptibility to fungal infection.
So, tissue and blood vessel damage from Covid-19, corticosteroid treatment, high levels of diabetes in the population most affected by the coronavirus and, most importantly, the most widespread exposure to fungi in the environment are factors of the situation we are seeing in India.
Challenges of treatment
In many western countries, increasing cases of another Aspergillosis fungal infection have been reported in patients with severe symptoms of Covid-19 who needed intensive care and were taking corticosteroids. This mushroom is also found in the environment but belongs to another family.
While Aspergillosis is the most common opportunistic fungus worldwide, and there are tests to quickly diagnose this infection. But this is not the case with mucormycosis. About half of the affected patients are likely to die and many of them will have permanent problems, reports abcnews.al
Timely diagnosis and intervention is very important. This includes controlling blood sugar, urgent removal of dead tissue, and treatment with antifungal medications. But unfortunately, many infections are diagnosed late and access to treatments is limited. This was the case in India before Covid-19 and current health system requirements will only make matters worse.
Controlling these fungal infections will require increasing the number of better tests to diagnose them in time, as well as focus on controlling diabetes and using corticosteroids properly. Patients should be operated on in time and treated with antifungals.
But there also needs to be more research on preventing these infections. abcnews.al